
EverCare
Companionship that cares
Brief
Rethinking Elderly Care with AI Companionship and Support
Objective:
The objective is to create an empathetic, accessible, and personalised digital companion that improves the emotional, social, and cognitive well-being of elderly residents while supporting caregivers and families.
Context:
The aged population is increasing worldwide, with a growing number of older adults residing in care home settings or living independently in their own communities. Older adults face many debilitating issues, such as loneliness and isolation, as well as memory impairment; this is particularly true for the growing number of older adults experiencing dementia or cognitive decline.
Care settings offer important physical supports to older adults but often lack the long-lasting and consistent physical companionship and social engagement that support their overall well-being. Families often feel they cannot connect meaningfully as often as they could, and caregivers themselves are stretched too thin to offer their full support in one-to-one interactions with older adults.
Current technology specialists have developed more accessible voice-activated assistants or companion robots to support too many older adults living alone today; however, many tend to lack cultural personalisation, accessibility in communities, and, ultimately, the robust integration of support with caregiving for the family and community.
Clearly, there is a need for a solution that connects older adults not only with reminders but also through emotional support, companionship and a lasting meaning in a simple and, ultimately, empathetic way.
🔍 Discover
Initial Research
Understanding the challenges of elderly individuals living in assisted living facilities or care homes is not only an important process, but it is a major issue that needs immediate action. Older adults are often ignored in society because many are simply unable to convey their needs due to physical limitations, cognitive decline, or mental health issues. Without being able to call out for help, these gaps in care and emotional well-being can remain present.
We require a compassionate understanding of this issue, but we need to identify what the lived experiences of elderly individuals are first. Preliminary data, suggest the difficulties that elderly individuals face are not confined to independent or isolated issues but instead, older adults are going through persistent struggles throughout practically all areas of life-from loneliness and solitude, to lack of effective communication, to mismanagement of health care, and the perception of dignity and independence.
The goal of this project is to identify, highlight and bring awareness to these struggles and ultimately, to find helpful ways to address, or contribute to addressing them through meaningful and thoughtful, human-centered design/approach.
https://www.figma.com/board/QQmMiTQEOYUHsCpIRT7LTu/Research-Board---Elderly-Companion?node-id=42-256&t=oCmLfyTHX19DQucI-4(Berg, 2022)
The first point of focus was on care homes (or nursing homes in the UK), which is completely relevant to issues facing UK society, because a significant number of elderly people live particularly in care homes. Care homes are part of the care system in this country and worldwide. Old people have spent their lives working and now and should be able to feel comfortable, happy and safe. This is true for the care homes, although there are issues which the elderly become increasingly exposed to with age, be it physical illness or mental health problems. Physical illnesses can be treated (or managed) medically, whereas mental health problems (for example, dementia and loneliness) are areas of care and support that specifically the individual needs care for.
In many cases the elderly adults in care homes, do not receive sufficient personal attention in the environment of a care home, as sadly we are unable to provide enough staff to assist the required level of personal support. Therefore, many elderly residents, do not get enough communication or social interaction with either caregivers or individuals as the staff are so stretched out providing majority of their shift taking care of the residents that they are run ragged with not enough staff and care to provide the service, support and care the individual should be provided with, which causes the elderly to feel sometimes isolated, and neglected emotionally.
Discovery Phase Objectives
Understand User Needs
- Explore the daily lives, challenges, and priorities of older adults in care homes and independent living.
- Identify pain points around loneliness, routines, memory, and accessibility.
Map Care Context
- Investigate how care staff and families currently support residents.
- Understand where gaps exist in emotional, social, and practical support.
Explore Cultural and Personal Preferences
- Learn how traditions, language, and personal history influence engagement.
- Identify opportunities for personalisation that feel meaningful.
Assess Technology Comfort Levels
- Evaluate how older adults interact with digital tools.
- Identify barriers such as trust, usability, or confidence.
Benchmark Existing Solutions
- Research current technologies designed for older adults (voice assistants, health apps, robotic aids).
- Highlight gaps and opportunities for differentiation.
Define Success Criteria
- Establish what a positive outcome looks like for residents, caregivers, and families.
- Align goals around emotional well-being, usability, and sustainability.
Possible Questions to be addressed
- How to support someone who is beginning to develop dementia?
- How to alleviate boredom for older adults living alone/care home?
- How to assist older adults with reminders to take their medications?
- How to assist older adults with feelings of loneliness?
- How to assist older adults with recollections of good times in their lives?
- How to make people feel like they are not mentally away from their family?
- How to let them experience positive moments with children/grand children?
Challenges facing by Elderly People
Loneliness & Social Isolation
- Many older adults lack regular social interaction.
- Emotional well-being is often overlooked in care settings.
Memory & Cognitive Decline
- Dementia and other impairments make it difficult to follow routines.
- Reminders need to be simple, clear, and supportive.
Accessibility Barriers
- Vision, hearing, and mobility issues limit how digital tools are used.
- Interfaces must be highly accessible with minimal complexity.
Technology Adoption
- Some older adults feel intimidated or unfamiliar with technology.
- Building confidence and trust is essential.
Personalization Needs
- Users come from diverse cultural, linguistic, and personal backgrounds.
- Generic solutions often fail to resonate or engage.
Caregiver & Family Involvement
- Families may be distant or busy, limiting meaningful connection.
- Care staff have limited time for individual attention.
Privacy & Trust
- Sensitive personal and health information must be protected.
- Users should feel safe and in control of their data.
Long-Term Engagement
- Sustaining interest and interaction over time is difficult.
- Risk of technology being abandoned if it feels irrelevant.
Problem Statement
Elderly people who reside in assisted living and care homes often have a myriad of unmet physical, emotional, and social needs. Owing to conditions commonly associated with aging (e.g., mobility limitations, cognitive decline, and difficulties communicating), many elderly individuals are not able to get the help and support they need. As a result, elderly residents may not receive the level of care and attention, or interaction they need for their overall well-being.
These issues influence a myriad of challenges beyond medical distress. Residents commonly experience challenges due to loneliness, inability to connect with meaningful engagement, increasingly dependent situations, and experiencing neglect. A care staff's intentions are typically very noble; however, high employee turnover and insufficient staff hours, traditionally limits the personalized attention and engagement an elderly resident can receive particularly at any designated time. Unfortunately, what results is a gap between the requisite quality of life older adults require by virtue of their age, and the care currently available to provide for them.
Addressing issues related to the care of elderly individuals, demands a compassionate, human-centred approach using empathy that seeks to not only honour the struggles of elderly residents, infuses meaning to support their dignity, independence, and emotional well-being while engaging with elderly residents based on need, wants and desires inside of care organizations.
Initiatives in Northern Ireland
Digital Adult Mental Health campaign launched
A new Digital Adult Mental Health and Wellbeing campaign has been launched to provide self-help resources and tools for those seeking support (Department of Health (Northern Ireland) 2024). Backed by the Department of Health and Digital Health & Care NI, the campaign features a range of mental health and wellbeing apps in the HSC Apps Library, covering topics such as anxiety, depression, stress, sleep and meditation.
Launched at the NICON conference, Health Minister Mike Nesbitt said the initiative shows how digital innovation can provide timely, accessible support, offering greater choice alongside traditional services. He highlighted the shift from analogue to digital healthcare as a key step towards better outcomes.
Community Mental Health Teams (Older People)
Community Mental Health Teams for Older People (CMHTOP) provide a Trustwide service from four Northern Trust localities. CMHTOP provides a service from 9.00am – 5.00 pm, Monday to Friday excluding Bank Holidays (Northern Health and Social Care Trust).
📖 Define
Drawing on the discoveries from the Discover phase, the aim of define is to synthesise the research into an understandable narrative about the core problems people living in elderly care are facing. While the discover phase initially surfaced their unmet physical, emotional and social needs, defining their problems will hone in on specific, well-defined problem areas, recognizing broad areas of challenges that can be targeted by design interventions.
In summary, the define phase will focus on building user needs, finding patterns in the research, and identifying pain-points that impact the quality of life of elderly people. This will also involve generating targeted problem statements and user insights that will ground the ideation and potential solutions moving forward. The define phase ultimately provides a process to ensure that the design process is evidenced-based, empathetic and grounded in the lived experience of elderly residents and caregivers.
Empathy Map
The Empathy Maps developed for Mary Thompson (Elder Resident) and Sean Maguire (Caregiver), were essential in shaping the future direction for the project. The Empathy Maps elucidated what each stakeholder thinks, feels, says, and does, and provided a more holistic understanding of each stakeholder's positions, emotions, and unfulfilled needs.
Mary Thompson (Elder Resident Empathy Map)
Mary's map explicated her feelings of being alone, her feelings of frustrated memory loss, and her quiet (yet real) desire to have human companionship and carry herself with dignity. Each were important because they illuminated her subsequent struggle with, and situated, technology, trust, and accessibility. By capturing Mary's feelings, the project was able to shape the value of simplicity, emotional connection, and confidence in potential solutions that supported, rather than overwhelmed, Mary as a stakeholder.Sean Maguire (Caregiver Empathy Map)
Sean's map centred on the agony of time, the guilt of being unable to meet the individual needs of residents, and the struggle of integrating physical and emotional care. By better understanding Sean's perspective, there was the potential to find opportunities in terms of solutions to lessen workload, free-up communication, and to create moments for useful relations with residents.The empathy maps were representative of what it is like to live in Mary’s world or to serve Mary in Sean’s world. The empathy maps were, essentially, mirrors of reality; if the future directions were to be realized, they would spring from a human need.
User Persona
To gain a deeper understanding of the experiences and needs of stakeholders in elderly care, four personas were produced: Mary Thompson (elderly resident), Sean Maguire (care worker), David O’Connor (family member), and Dr. Priya Varma (healthcare professional). The purpose of generating these personas was to synthesise the research findings and provide a people-centred perspective from which the project could continue. The process to create these personas was underpinned by secondary research, stakeholder interviews, surveys and empathy mapping to ensure the design direction was evidence-informed and user-centred.
Contribution to the Define Stage
The personas were a crucial tool for the Define phase of the Double Diamond process, summarizing the research findings while framing the central challenges:
Highlighting needs
Elderly residents want companionship and emotional support.
Care workers want efficiency and relief from the workload.
Families want trust, reassurance, and transparency.
Healthcare professionals want safety, reliability, and ethical standards.Problem Definition
The personas enabled the articulation of human-centered problem statements like:
How can an AI companion alleviate loneliness for residents, while enhancing, rather than replacing, human care?
How can technology help staff to deliver quality care, while maintaining, or not adding to their workload?
How can families stay informed and maintain an emotional connection to loved ones when they are unable to be there physically?
How can we design our innovations with regards to ethical, clinical, and privacy considerations?
Stakeholder Alignment
The personas showed common ground across concerns (i.e. loneliness, time, reassurance) and supported alignment on project objectives on the basis of empathetic, trustworthy, and practical AI interventions.
The persona usage was reassuring and provided a focused exploration of user needs; an efficient hand-off from published research findings to meaningful design challenges was established. The Define stage was able to refine and capture particular problem statements, and bring together stakeholders so the subsequent ideation and prototyping stages were based in empathy, pragmatism, and ethical stewardship.
Interviews
The discussions with care staff members and various family members fully support what I’ve already heard from the residents - when there are structured group activities, such as music therapy and exercise, or meals, this is beneficial for those residents who participated. In addition, inactivity and quiet times, especially in the afternoon, will also commonly again happen, generally when their mood is not as good, or mood and withdrawal are more pronounced, and loneliness is elevated, especially for residents whose family has only come one time, or at most a few times. Irrespective of time, gestures of intimacy, or conversation, or calm reminders do impact the resident's involvement and emotional state.
Residents with some cognitive decline, or dementia will need a number of gentle reminders, listed down for their meal routines day to day, as well medication and socialising with others. Although there are some familiar and visual aids which provide some help in care facilities, a busy care staff member on any given day can have up to 5 people to help them at meal time, for example. This unfortunately limits support, and whether staff have time to take someone - if they can only deal with one person.
Care staff are pulled in many different directions and families struggle with distance and limitations on their schedule to support on a regular basis. Digital solutions can offer a way to enhance what staff are able to do, enhance the connection with family and friends and offer some social engagement that is personalized for residents, including reminders, conversation and mood-aware interaction.
In summary, these insights speak to a clear need for solutions that enhance emotional, social and cognitive support, reduce isolation and help both residents and caregivers take charge of shared care.
User Journey Map
The turning point of the journey map from the elderly residents demonstrates a routine that appears to be structured, however, it is often repetitive and ends up causing feelings of isolation, forgetfulness, and low stimulation. Social points, such as meals or tea breaks, provide some small reprieve, however, they are usually brief and limited, and residents are left by themselves vulnerable to isolation and disconnection, particularly between the late afternoon hours on quote/unquote “twilight’’ as well as through the evening and nighttime.
There are key pain points in the map: forgetfulness and disorientation, continuous repetitiveness, and loneliness has peaks at evening time. There are many opportunities: increasing more engaging small moments of activity, social moments at mealtimes with improved facilitation, using memory prompts and reminders, and developing calming rituals at nighttime.
At the end of the overall big picture, the general insights were that residents require consistent stimulation, companionship, and soft guidance at points throughout the day. Addressing stimulation, companionship, and guidance with the residents could create significant opportunities to improve wellbeing and promote an environment that reduces feelings of isolation.
Problem-Solution Analysis Report
Through a problems tree analysis, we analyzed the challenges encountered by older adults in care environments, associated causes, consequences, and possible solutions. We identified these opportunities and aligned them with current practices to identify gaps that solutions like EverCare could fill.
Key Insights
Social Isolation and Emotional Needs
- Root Causes: Distance from families, limited time for staffing considerations, lack of culturally appropriate strategies or emotional awareness.
- Consequences: People are lonely, losing routines, and putting strain back on staff.
- Interventions: Using AI - prompted companions for social interaction and reminders (not fully established so requires pilot testing), culturally adaptable engagement activities, and tools to enhance family connection.
Difficulty Following Routines and Medication
- Root Causes: Cognitive functioning and signage limitations, possible lack of structure or reminders procedures.
- Consequences: Missed medications, health risks increasing, and dependence dwindling.
- Interventions: Smart reminders (AI- or phone-based), staff-assisted check-ins for medication or nourishment, and modelling/habitually reinforcing individualized behaviours.
Sustaining Engagement Over Time
- Root Causes: Not enough variability in activities; no cultural inclusiveness.
- Consequences: Residents will disengage, have less cognitive stimulation, and enjoyment.
- Interventions: Rotating group activity programs, events with culturally relevant content, and digital apps for reminiscence therapy.
Limited Staff Time for Individual Attention
- Cause(s): High staff-to-resident ratios and complex schedules
- Impact(s): Residents' needs may not be met in a timely manner, staff may experience fatigue.
- Solution(s): AI-powered assistants as reminders and companions, prototyping volunteer programs for companionship.
Opportunities.
While many prototypes such as reminder applications, digital forms of therapy, or AI companions like EilliQ exist, there is spontaneous, disjointed use.
AI Companion could provide benefits through:- Fully integrated, experiential AI supportive functions that offer procedural and emotional support (reminders, routines).
- Support cultural and cognitive diversity
- Reduce staff "to-do's" while increasing a sense of independence and belonging for residents.
Conclusion
The analysis above highlights that older adults are dealing with interrelated challenges related to memory, social connection, and limited availability of caregivers. EverCare could become the new way to identify ways to connect the dots. An AI powered "all-in-one," comprehensive support system that ensures care that is continuous (around the clock), personalized, and emotionally supportive.Potential solutions for the problems facing by Elderly People who lives in assisted facilities
Elderly residents in assisted living and care facilities may encounter challenges related to feelings of loneliness, cognitive decline, loss of independence, and limited social interaction. This next step to identify options for resident involvement needs a human centred design process, including gathering input from residents, caregivers, family, and health care providers. This report summarizes the potential interventions and technological innovations and improvements available to improve quality of life and emotional well-being based on care experiences to enhance care efficiencies in assisted living environments.
AI-Powered Companions and Social Robots
- Provide conversation, entertainment, and reminders to reduce loneliness.
- Offer cognitive stimulation activities such as quizzes, memory games, and virtual storytelling.
- Act as a non-intrusive presence to provide reassurance during periods of staff unavailability.
Digital Communication Tools for Families
- Video call systems or secure apps to connect residents with family members.
- Updates on daily routines, health metrics, and personalised messages to improve trust and engagement.
Personalised Care Plans Supported by Technology
- AI-assisted scheduling to optimise care staff allocation.
- Wearable devices to track activity, sleep, and vital signs, ensuring timely interventions.
Cognitive and Physical Stimulation Programs
- Virtual reality or tablet-based activities for mental stimulation.
- Group activities, interactive workshops, and adaptive exercise programs to promote socialisation and physical wellbeing.
Environmental and Sensory Enhancements
- Smart lighting, calming soundscapes, and interactive ambient features to improve mood and orientation.
- Personalised room settings to give residents a sense of autonomy and comfort.
Caregiver Support Systems
- Dashboards and alerts to help staff monitor resident wellbeing efficiently.
- Training tools for staff to manage cognitive impairments and emotional support effectively.
Effectively responding to the challenges encountered by older residents living in their care environments takes a combination of emerging technologies, person-centred care, and social connectivity opportunities. The promise of: AI companions, virtual connectivity, cognitive/physical enrichment, better environmental standards, and amenities can enhance overall quality of life, reduce dependence, and relieve essentialist workloads from care workers. These are a foundation of humane centred care solutions that are ethical, compassionate and realistic.
Competitor Analysis Report
AI and robotics companions for aging-in-place care are demonstrating promise and potential, but each of the current products has its own pros and cons. For example, while both ElliQ and PARO demonstrated strong evidence of impact, they were both constrained on accessibility (ElliQ with ongoing subscription and connectivity requirements; PARO is expensive with little therapeutic function beyond therapy).
Other products like AvatarMind iPal and Hyodol widen the scope with socialization, safety, or culturally designed dementia companions, but they are limited to adoption by unclear clinical outcomes, maintenance of the robotic capabilities, limited marketing reach, and ethical issues around privacy and authenticity.
So, although there were some promising products, the failures of alternatives also demonstrated limitations of the current market and, while some products excelled in therapy effectiveness, others were able to provide social engagement or monitoring without posing a clear multi-function alternative. In brief, we see an opportunity for a more companionable AI that is publicly affordable, easy-to-use, functionally sound, with transparent ethical data and privacy protocols that offers therapeutic value as opposed to practical value at the time of traumatic, nostalgic, or convenient use for older adults and their caregivers.
❓HMW
Multiple 'How Might We' (HMW) questions were generated during the study, which were subsequently synthesised into a single, comprehensive HMW statement to guide the project.
“How might we support older adults in care by reducing isolation, assisting with routines, and creating meaningful, culturally relevant engagement, while also easing the burden on families and care staff?”
How might we help older adults maintain regular social interactions even when families are distant or staff are busy?
How might we create meaningful connections between residents, families, and staff despite time and distance constraints?
How might we support residents with dementia or impairments in following daily routines more easily?
How might we ensure older adults remember to take their medication on time without overwhelming them?
How might we reduce the burden on care staff while still ensuring residents feel attended to individually?
How might we assist careworkers in responding to resident needs promptly even with a busy schedule?
How might we design activities that sustain residents’ interest and engagement over time?
How might we adapt engagement to suit diverse cultural, linguistic, and personal backgrounds?
How might we incorporate cultural traditions, festivals, and storytelling into daily care experiences?
How might we enable residents to reminisce and relive memories in a way that strengthens emotional wellbeing?
🛠️ Develop
Ideation: Introducing EverCare
The Name: EverCare
When searching for our name we thought of many possibilities, but when we discovered "EverCare" we stuck with it, because it has timeless meaning. "Ever" implies continuity, something that will be in place for ever, while "Care" is about compassion, support and wellbeing. Combined, they promise "care that never ends." With Artificial Intelligence as the core of EverCare, support, companionship, and attention will always be present bringing peace of mind to residents, families, and caregivers that care truly lasts forever.
EverCare: Companionship that cares
EverCare is an AI-enabled companion designed to aid elderly residents of assisted living and care facilities. It provides a solution to problems related to loneliness, cognitive decline, and decreased independence. In addition, it provides emotional and practical support where gaps in timely or human support exist. In this ideation phase, we seek to generate creative and human-centred solutions that use AI to improve residents' wellbeing, support care workers, and support more meaningful connections with family.
Following research, stakeholder interviews, and the development of personas, this phase seeks to explore solutions for AI companionship, patron usability, cognitive engagement, and interactive stimulation. The goal for this phase is to convert the needs and challenges defined above into concrete potential ideas, while ensuring that EverCare is empathetic, trustworthy, and ethically sound in providing a better quality of life for elderly residents, and those who support them.
Feasibility Survey
Survey Summary: Family & Caregivers’ Views on AI Companions for Elderly Residents
The survey was distributed to family members and caregivers to investigate the potential use of AI companions to assist elderly residents. Nine responses were collected from family members and caregivers about this possibility.
Openness to AI
- All of the respondents were receptive to the idea with the results as follows: 6 Yes, 2 Maybe, and 1 No.
- This is interpreted positively as a general openness to the possibility of exploring AI as a support tool.
Perceived Benefits
- Survey participants specifically mentioned the value of AI as:
Friend - Reducing isolation (through conversation).
Cognitive stimulation - Quizzes, games, storytelling.
Health & safety reminders (e.g., medication, meals, routines).
- While families considered AI as potentially one option in their continuum of care by providing companionship and structure.
Concerns Expressed
- The most common concern was ease of use, and 3 participants mentioned it could be too complex to use.
- Others spoke to the dangers that families would become too reliant on, or would replace, human contact and the need to retain human relationships would be taken away.
- That said, they did cite privacy issues related to the sharing of data, but that was considered a secondary concern.
Trust and Reassurances
- Respondents commented they would expect to trust an AI companion, if they confirmed privacy of data, transparency about data use, etc. and the AI had been adequately tested.
- There were mixed opinions about emergency alert features; 3 supportive, 3 unsure, and 3 against - showing that caution and control in framing would be required in this space.
Overall Feasibility
The findings indicate that families and caregivers recognized the potential in using AI companions for older human residents, mostly for the purposes of diminishing loneliness and assisting with routines. However, feasibility relies on:
- Designing an interface that is simple enough to be intuitive.
- Protecting privacy, transparency and reliability.
- Portraying AI as a support companion option, not as a replacement for a human care.
Userflow
The user flow begins with a detailed step-by-step onboarding that assists users in creating an account, setting accessibility settings, and customizing their AI companion. After onboarding, users will arrive at Home, which has an uncomplicated tile-based interface for easy navigation.
From Home screen users can access the core features to easily:
Daily Routine & Medicine Reminders for structured support.
Smart Device Control to gain access to connected devices.
Media & Entertainment for stimulation and engagement.
Communication to communicate with family and caregivers.
Wellness & Mental Health features for emotional and mental support.
Emergency & Support to provide quick access to urgent support.
Settings for personalization and setup.
This flow will allow for easy onboarding and a centralised, intuitive hub for all key features with minimal requirements from the user.
User Account Types
- Resident / Elderly Person
- Caregiver
- Family / Friends
- Administrator
Feature Overview
The EverCare platform is built to support older adults in assisted living and care facilities with functionality guided by Artificial Intelligence and to do so comprehensively. To create a solution that can work to meet the needs of all parties involved, both directly and indirectly in facilitating care, a comprehensive feature set has been built for four areas of users: Residents, Caregivers, Family/Friends, and Administrators.
This part presents the core and enhanced functionality available for each user type, developed from research, stakeholder interviews and persona analysis. Functionality will differ for each of the users, with features including AI companionship, mood tracking and reminders for residents, dashboards, analytics and communication for caregivers, family and friends, and reporting, security and communication for administration. The functional aim of the feature set is to improve the wellbeing of residents, assist caregivers with personalization in care, improve family connection, and support comfort and security of facility management.
Resident / Elderly Person (User Type)
- Voice Assistant / AI Companion
- SOS / Emergency Alerts (with location tracking)
- Call Care Staff
- Video Call with Family or Caregivers
- Reminders & Routine Support (medication, appointments, daily tasks)
- Mood Tracker (AI-driven)
- Games & Cognitive Activities
- Ambient Mode (Emotion-driven environment adjustments)
- Quick Wishes / Messages to Family or Staff
- Music & Entertainment
- Messages / Notes
- Smart Home Connectivity (lights, temperature, etc.)
- Health Monitoring (vitals, sleep, activity)
- Accessibility Settings (font size, contrast, voice speed, language options)
- Medication Reminders & Tracking
Caregiver (User Type)
- Resident Dashboard (overview of health, mood, and activity)
- Quick Emotional Reports / Mood Analytics
- One-Tap Broadcast / Video Message Tool
- Task Manager & Alerts (care tasks, reminders, emergencies)
- Resident Profile (medical info, preferences, notes)
- AI Suggestions / Recommendations (engagement, care tips)
- Voice Notes / Care Logs
- Shift / Schedule Management
- Alert Prioritization / Filtering
- Analytics / Trend Insights (resident wellbeing over time)
Family / Friends (User Type)
- Video / Voice Call (with scheduling)
- Mood & Well-being Feed
- Memory Upload (photos, videos, messages)
- Milestone Notifications (birthdays, anniversaries, achievements)
- Messaging / Notes to Caregivers
- Quick Wishes
- Consent Management (control what information is shared)
- Activity Suggestions (AI-recommended engagement ideas)
- Shared Calendar for Visits / Calls
Administrator (User Type)
- Resident Dashboard
- Quick Emotional Reports / Mood Analytics
- One-Tap Broadcast / Video Message Tool
- Alerts & Notifications
- Resident Profile Management
- Accounts Management (staff, residents, family)
- Security Management & Access Controls
- Compliance / Audit Logs
- System Analytics (usage stats, resident engagement metrics)
- Staff Management & Permissions
User Journey Mapping
The map illustrates the day-in-the-life journey of an individual older adult user of the AI companion (EverCare). Specifically, the following areas are captured:
Stages: Morning wake-up → daily activities → emergencies → preparing for sleep;
User goals: what the resident wants to accomplish at each stage (e.g., "I want to wake up on time," "I want to unwind", "I want to relax before sleep");
Actions: what the AI does to support (e.g., reminders, activity suggestions, emergency detection);
Thoughts & Feelings: emotional responses (e.g., "It feels nice to be asked", "I feel safe");
Pain Points: challenges without support (e.g., taking medication, loneliness, complacency in emergencies);
Opportunities for AI Companion: how EverCare can assist to minimize pain points (e.g., voice greetings, passive monitoring, personalized conversations).Empathy & Understanding:
Journey map helps to cultivate a deeper understanding of the residents' experiences, including their individual routines, challenges, and emotional highs and lows.
Seeks to flip the lens away from medical needs toward emotional and social health.
Feature Prioritization:
Clarity in mapping the pain points to the opportunities informed where features could be prioritized (medication reminders, mood check-ins/emotional support, emergency alerts).
Ensure the features were not solely tech-driven but evidenced user needs.
Design Alignment:
Grounded the design of the Resident Dashboard to reflect where caregivers and family members need visibility (missed meals, mood, emergencies).
Helped determine and set notifications imagined for different time periods of the day.
User Experience Consistency:
Provided the process with a path to ensure that the AI companion will provide gentle, supportive and contextual interactions during the day within user experience interaction patterns.
Provides a holistic experience anchoring the residents' goals and feelings during the interactions to ensure experience is not fragmented.
Communication with Stakeholders:
Provides a story in a clear visual communication to help explain why particular features are valuable (e.g. loneliness → evening companionship feature).
Connected ecosystem of EverCare AI Companion
This Ecosystem illustrates the "EverCare" AI companion system which, as a connected ecosystem, is designed for the room of an elderly resident. At the center of the system is a single Network / App Server, acting as the command center for linking together all of the system's devices.The primary device used by the resident is the Central Device; a tablet encased within a photo frame, housing the Elderly Companion App, and serving as a voice assistant offering audio feedback, while also providing visual interactive content.
Optional Co-Pilot Devices, such as a Smart Remote and and a Smart TV, illustrate the flexibility of the Central Device and allow a resident opportunity to communicate with different devices from different locations, but also provide access to the features of the app in new ways - e.g. video calling on the Smart TV screen.
The system also offers Smart Home Integration. An adjustable smart light - controlled using the AI companion - illustrates how EverCare can lead to a more comfortable and responsive environment.
In summary, the diagram illustrates a centralized, AI-driven coordinative system that employs a network server for managing multiple devices to provide the resident with an individualized, linked, and supportive living space that can deliver voice controlled assistance, communication, and control the environment.
Wireframe / Mid-Fi Prototype
The mid-fidelity prototype included the signup process, landing pages for the platform and tasks, and what the interfaces would look like for families and caregivers. I didn't do low-fidelity wireframes because I had a thorough understanding of the user needs, personas, and a set of core tasks (research already did that part) so the next part could focus on interaction flows, as well as layout (making it clear and accessible for elderly users), while still enabling good usability testing and enough opportunities for iterative design modifications.
Protype Link : https://www.figma.com/proto/PLMcGGAdv1UU6dTRqGYPk0/App?node-id=0-1&t=UbC6lUnKyq7bCiOJ-1
✅ Deliver
Branding
The EverCare logo expresses the project's spirit of caring, continuous care. The design includes an outlined care worker's figure that has an abstract torso and head shape that resembles a heart shape that represents the AI's care and empathetic nature. The arc shape resembles infinity, to symbolize that the care is carried on, it is abiding, or "ever" care for the elderly and their families, such that even the emotional and practical support we deliver to elderly residents and their families is consistent and "ever" present.
Thus, the human form with heart, at the same time indicates trust, empathy, and continual commitment, while providing clean and simple styling as a design for print or digital format.
Logo
The EverCare logo represents the project's purpose of compassionate, continuous care. The design employs an outlined form of a care worker in which their body also suggests a heart, reflecting the care and compassion of the AI. The flowing outline can also be read as the infinity symbol, relating to care that is uninterrupted, permanent, and "forever," as relates to EverCare's vision of continuous emotional and practical support for older adults.
This hybrid of human figure, heart, and infinity conveys a notion of trust, compassion, and timeless dedication, while still being a crisp, adaptable logo for various digital and print contexts.
Color Palette
WCAG Contrast Compliance
The EverCare color palette was chosen not only for visual consistency but also for accessibility with the app’s UI. The component colors for EverCare include primary, secondary, tertiary, success, and background color. Each color, was contrasted at the time of selection and approved based on WCAG compliance.
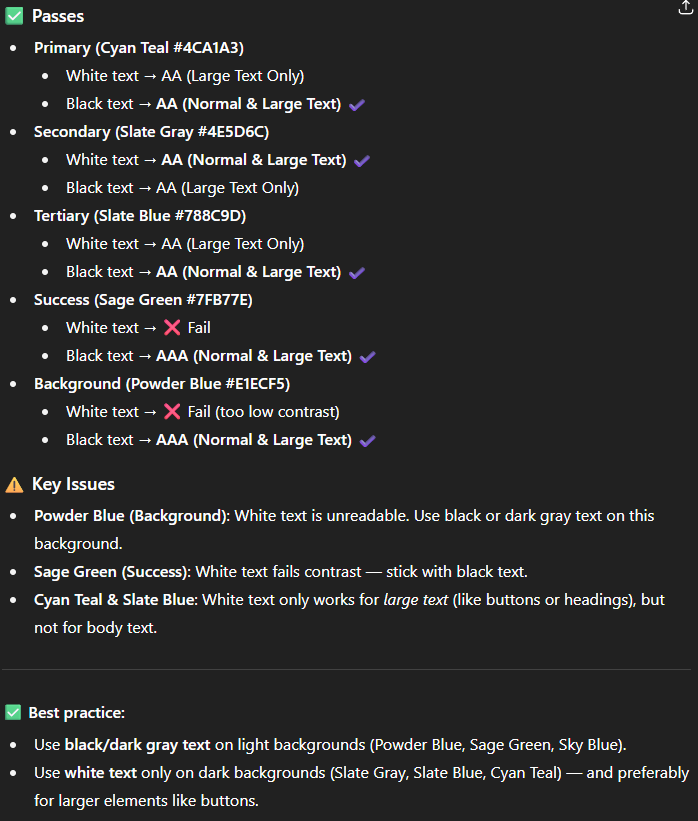
Some colors did fail to pass with white text during the WCAG compliance testing, although the colors were not utilized in those combinations in the UI. Overall the palette strikes a good balance between being accessible and visually harmonious with regard to the intended calm, supportive feel of the app.
User Interface / Design System
This app includes custom buttons and layouts specifically targeted at accessibility for older people. The app is focused on voice over touch and contains a small number of screens, so at this stage, a full design system is not required.
Brand Experience Guide
https://www.figma.com/proto/0i1j7KZeYQiggrOuw35hLE/Branding?node-id=18-39&t=XWgMvHYsAxJqTI6E-1
Final Solution EverCare App (Prototype)
The EverCare Figma prototype is tailored specifically for tablet and iPad devices, with a user-friendly interface that was carefully planned and designed for use by elderly users, caregivers, and family members. The Figma prototype reflects the findings of user research, the personas created, and other design iterations to ensure that the primary features of the app - reminders, video calls, activities, notifications, and support in an emergency - are prominently displayed to allow for ease-of-use and functionality.
Therefore, the prototype's design features clarity, accessibility, and interaction. The design includes large tap targets, large fonts for better contrast, and a simple layout that is suitable for a tablet screen. The prototype itself includes interactive features of the app like voice activation, prompts, reminders, and quick links for the user to engage with the app as experienced by the intended user.
Overall, the prototype should be viewed as a functioning representation of the EverCare app. It represents both the visual style of the app and the interactive user flows, and it is intended to be used for usability tests and further considerations for in-field implementation.
Usability Testing
Supporting Apps (for Caregiver & Family)
✨ Future
Future of EverCare

An EverCare app installed ipad (in a photoframe case) standing on table
EverCare has been intentionally designed to be an affordable, easy-to-use digital solution for improving the well-being of elderly residents in a care setting, while also supporting their caregivers and family members. EverCare's long-term goal is to be an affordable tool for existing users, and transform into a scalable, fully integrated, smart eco-system that can accommodate future emerging technologies, and more importantly, the evolving needs of users.
Growth and Accessibility
One of EverCare's primary advantages is that it is affordable. This allows many more people to access EverCare from families, care homes, and individual users. Affordability will also shape the future growth of the app to expand into broader markets in the UK and beyond. As demand for digital health care continues to grow, EverCare can emerge as an accessible, trusted, mainstream digital platform for elderly care and well-being support.
Smart Home and Device Integration
Moving forward it is anticipated that EverCare will be integrated with leading smart home ecosystems, such as Amazon Alexa, Google Home and Apple HomeKit. Such integrations will allow older persons or their caregivers to use voice commands for EverCare features, making it less of a barrier for users with impaired mobility or dexterity.
EverCare will also pursue integrations with other smart devices, such as:
Smart TVs - to facilitate the ability to do a simplified video call, an important area for the older person + reminders and wellbeing updates, on larger screens.
Music Systems - to provide lists of mood music, or cognitive therapy through sound and music with users.
Smart Lighting - to change lighting levels in user rooms according to routines, mood or wellbeing needs
Such connectivity will increase the users' and caregivers' sense of connectedness and supportive environment, Eisenbahnsulating the extent to which EverCare becomes an inherent part of daily living, and functionality is considered normal.
Integrations with Connecting Health Ecosystem
Future developments will include extensibility with electronic health records (EHR's) and care management systems. By collaborating with NHS Digital initiatives and local care management platforms, EverCare could provide real-time and extensibility opportunities to share information between older persons and health care providers that are both proactive and personalised.
AI and Personalisation
AI (artificial intelligence) will increasingly play a role in EverCare as it continues to develop. By accessing and reviewing information regarding user interaction, preferences and health data, the app will be able to assess personal needs and provide suggestions, daily wellbeing reminders, and potentially, early recognition of concerning behaviour relating to mood, sleep or patterns of activity. In this way, EverCare will reinforce its value as a care resource and support preventative health actions.
Global Scalability
Ultimately, EverCare could scale and move into global markets by adapting and contextualising features, while maintaining its core principle of accessibility and inclusivity. Through partnerships and relationships with local health organisations, government institutions, and NGOs, EverCare likely could continue to provide supports related to elderly care on a global scale.
A sample conversation (voice) between EverCare Companion and Elderly resident Conclusion
The success of EverCare, ultimately, is its ability to develop into a holistic, integrated platform that provides support for elderly people, their providers, and families across varied dimensions of care. While affordability is the underpinning of EverCare, and incremental technological advances future the platform, there exists an opportunity for EverCare to change the way elderly care is provided, affording everyone the opportunity for compassionate, connected, and smart support.
References
- Berg, V. (2022) Care home stats: Number of settings, population & workforce. Available at: https://www.carehome.co.uk/advice/care-home-stats-number-of-settings-population-workforce (Accessed: 12 June 2025).
- Department of Health (Northern Ireland)(2024)
- Digital Adult Mental Health campaign launched. Published 16 October 2024. Available at: https://www.health-ni.gov.uk/news/digital-adult-mental-health-campaign-launched (Accessed: 28 June 2025).
- Freepik (no date) () . (Images used for the UI Design)Available at: https://www.freepik.com (Accessed: August 2025).
- OpenAI ChatGPT, 2025. Response to author's query, 12 May. (refine grammar, improve wording, and ensure adherence to the word limit in parts of this document.).
- South Eastern Health & Social Care Trust (no date)
- Community Mental Health Teams. Available at: https://setrust.hscni.net/service/community-mental-health-teams/ (Accessed: 25 June 2025).
